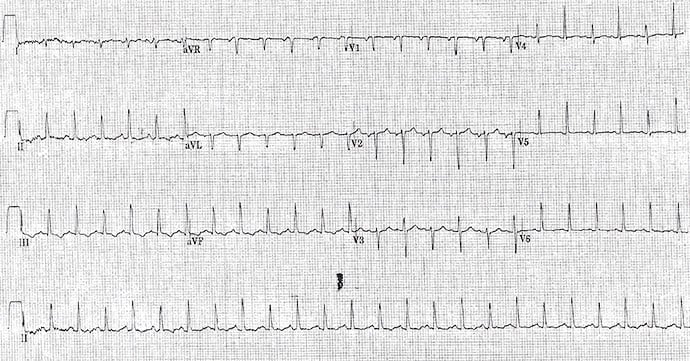
A 56-year-old woman who underwent recent coronary artery bypass graft (CABG) surgery for three-vessel coronary artery disease (CAD) presents for routine post-operation follow-up with complaints of fatigue, chest discomfort (unrelated to the sternal incision and seemingly not anginal), shortness of breath, and peripheral edema. A 12-lead ECG is obtained, and the findings are consistent with the physical examination and echocardiogram.
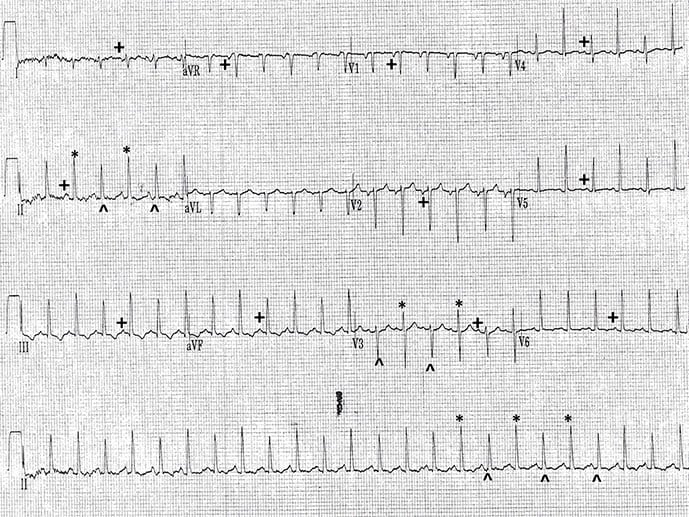
The correct diagnosis is sinus tachycardia with electrical alternans (Figure 2).
Discussion
The rhythm is regular at a rate of 130 beats/min. A P wave occurs before each QRS complex (+) with a stable PR interval (0.14 sec). The P wave is positive in leads I, II, aVF, and V4-V6. This is a sinus tachycardia. The P waves are negative in leads V1-V2, consistent with a left atrial abnormality or left atrial hypertrophy.
The QRS complex duration (0.08 sec) and morphology are normal. The QT/QTc intervals are normal (240/350 msec). The axis is rightward between +90° and +180° (negative QRS complex in lead I and positive in lead aVF).
Potential causes for a rightward axis include:
- Right ventricular hypertrophy: Associated with a tall R wave in lead V1 and often P pulmonale
- Wolff-Parkinson-White pattern: Short PR interval and delta wave
- Lateral wall myocardial infarction: Deep Q wave in leads I and aVL
- Right-left arm lead switch: Negative P and T waves in leads I and aVL, and positive QRS complex, P and T waves in lead aVR
- Dextrocardia: Appears as a right-left arm lead switch as well as reverse R wave progression in leads V1-V6
- Left posterior fascicular block: A diagnosis of exclusion when there is no other cause for the right axis noted
This is a case of left posterior fascicular block. Note the beat-to-beat changes in the QRS complex amplitude (*, ^); these are known as QRS or electrical alternans. Given the history and the presence of sinus tachycardia, the most likely cause for this is a large pericardial effusion or tamponade. Consistent with this diagnosis is P wave alternans, which is seen in lead aVR.
Other causes of electrical alternans include rapid supraventricular tachycardia, acute ST segment elevation myocardial infarction, dilated cardiomyopathy, or decompensated heart failure. However, P wave alternans is not seen in these cases of electrical alternans and is specific to a large effusion or tamponade.
Philip Podrid, MD, is an electrophysiologist, a professor of medicine and pharmacology at Boston University School of Medicine, and a lecturer in medicine at Harvard Medical School. Although retired from clinical practice, he continues to teach clinical cardiology and especially ECGs to medical students, house staff, and cardiology fellows at many major teaching hospitals in Massachusetts. In his limited free time he enjoys photography, music, and reading.

